Gastro-oesophageal Reflux (GORD) or Heartburn
Anatomy
A ring of muscular tissue (the lower oesophageal sphincter) at the junction of oesophagus (gullet) and stomach acts as a one-way valve. It allows the passage of food and liquid from the oesophagus into the stomach. It closes to prevent regurgitation of stomach content (such as acid and bile) into the oesophagus. When the sphincter fails to close completely the oesophagus will be exposed to the stomach acid, giving rise to gastro-oesophageal reflux disease (GORD) or heartburn.
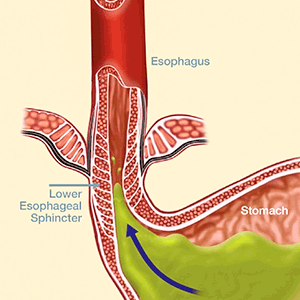
Lower oesophageal sphincter
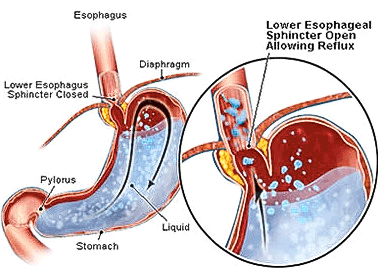
Reflux mechanism
GORD is also associated with a larger than usual gap in the hiatus or opening through which the oesophagus passes through the diaphragm. If the stomach pushes up through this gap into the chest cavity, a hiatus hernia is said to occur.
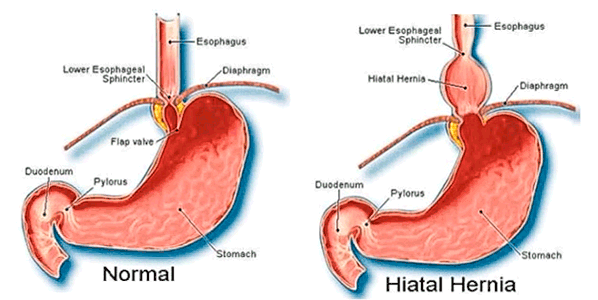
Hiatus hernia
GORD is a chronic condition. It may be complicated by:
- Ulceration and bleeding from the oesophagus stricture or abnormal narrowing of the oesophagus.
- Change in the oesophageal lining cells to a premalignant cell type (Barrett’s oesophagus). This may lead to oesophageal cancer.
- Oesophageal cancer.
Symptoms
GORD affects about 20–40% of adults.
The common symptoms include:
The common symptoms include:
- heartburn
- acidic taste in the mouth or back of throat
- difficulty in swallowing
- chest pain
- burning pain in the throat
- chronic cough.
Management
Simple reflux disease can be managed by:
Lifestyle changes
Typically, lifestyle changes involve eating and drinking habits.
Medications
Typically, patients are prescribed a group of medications called proton pump inhibitor (PPI). This group of medications reduces the amount of acid in the stomach, which would then reduce the amount of acid refluxing into the oesophagus.
Surgery
The aim of surgery is to augment the lower oesophageal sphincter, which cannot be corrected by medication.
Change in life style and medications do not address the underlying cause of GORD. There are also concerns about the effect of long-term medications. Recent studies have shown that surgery is also more effective in controlling GORD than medications.
Lifestyle changes
Typically, lifestyle changes involve eating and drinking habits.
Medications
Typically, patients are prescribed a group of medications called proton pump inhibitor (PPI). This group of medications reduces the amount of acid in the stomach, which would then reduce the amount of acid refluxing into the oesophagus.
Surgery
The aim of surgery is to augment the lower oesophageal sphincter, which cannot be corrected by medication.
Change in life style and medications do not address the underlying cause of GORD. There are also concerns about the effect of long-term medications. Recent studies have shown that surgery is also more effective in controlling GORD than medications.
Surgery
Gastro-Oesophageal Reflux Surgery
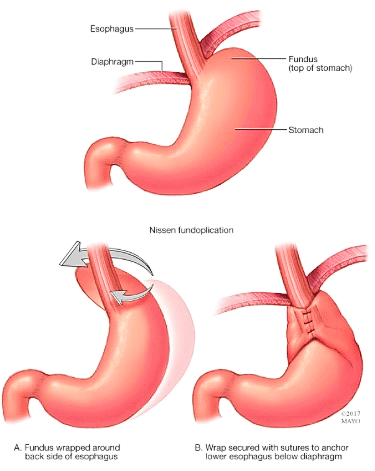
The aim of surgery is to augment the lower oesophageal sphincter by wrapping the top of the stomach around the bottom of the oesophagus or gullet, a procedure called fundoplication. There are a variety of fundoplications that are employed. These procedures are usually performed by laparoscopic (key hole surgery) and only occasionally by open surgery.
The commonest of these are:
The commonest of these are:
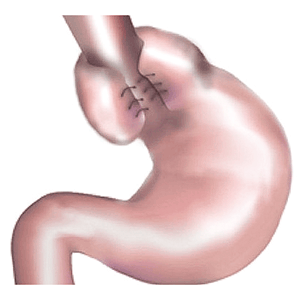
- Nissen fundoplication. In this procedure, the upper part of the stomach is wrapped completely (360º) around the lower part of the oesophagus.
- Anterior or posterior partial fundoplication. The upper of the stomach is partially wrapped (180º) around the lower oesophagus.
Nissen fundoplication
Posterior fundoplication

Anterior fundoplication
Laparoscopic Gastro-Oesophageal Reflux Surgery
In this procedure, the surgery is performed using a laparoscope (a small rod like telescope). This is inserted through a small incision in the upper abdomen. Operating instruments are then inserted through 4 small incisions.
The diaphragmatic crura (where the oesophagus or gullet passes through to be connected to the stomach) are dissected and defined. The hiatus hernia (if present) is dissected and repaired. Vascular attachments between the upper stomach and spleen are then divided. Suturing the diaphragmatic crura brings the diaphragmatic opening together. The upper part of the stomach is then pulled to encircle the lower oesophagus and sutured to itself (for a classic Nissen Fundoplication).
For a partial fundoplication repair, the upper part of the stomach is pulled across the front of the gullet and sutured to the diaphragm and sidewall of the oesophagus.
The diaphragmatic crura (where the oesophagus or gullet passes through to be connected to the stomach) are dissected and defined. The hiatus hernia (if present) is dissected and repaired. Vascular attachments between the upper stomach and spleen are then divided. Suturing the diaphragmatic crura brings the diaphragmatic opening together. The upper part of the stomach is then pulled to encircle the lower oesophagus and sutured to itself (for a classic Nissen Fundoplication).
For a partial fundoplication repair, the upper part of the stomach is pulled across the front of the gullet and sutured to the diaphragm and sidewall of the oesophagus.
Complications of laparoscopic gastro-oesophageal reflux surgery
These are uncommon (1%). The complication rates are higher in a patient who has had previous upper abdominal surgery.
Complications include those sustained during the operation such as:
Overall, 2–3% of patients will require further surgery due to complications specific to the procedure which include:
Complications include those sustained during the operation such as:
- Damage to the surrounding organs such as stomach, spleen and oesophagus. This may require an open surgery to repair the injury.
- Conversion to an open procedure (i.e. procedure through a big midline incision). This is associated with a longer postoperative recovery.
Overall, 2–3% of patients will require further surgery due to complications specific to the procedure which include:
- Increased flatus (gas).
- Difficulty in swallowing. This usually resolves in 3–4 weeks, without requiring surgery.
- A sensation of early fullness after meals. This tends to resolve in 9 out of 10 cases.
Postoperative management
Most patients will stay in the hospital for 1–2 days.
After recovery from the general anaesthesia, patients are allowed oral fluid.
For the first few weeks, patients are expected to eat soft food, but avoid gluggy absorbent food such as rice and white bread or solid food with long fibre or high fibre content such as steak, apples and peas.
Most patients should be able to commence normal daily living after 1–2 weeks.
After recovery from the general anaesthesia, patients are allowed oral fluid.
For the first few weeks, patients are expected to eat soft food, but avoid gluggy absorbent food such as rice and white bread or solid food with long fibre or high fibre content such as steak, apples and peas.
Most patients should be able to commence normal daily living after 1–2 weeks.
Clinical Associate Professor Hairul Ahmad MBBS FRACS
Upper Gastrointestinal, Advanced Laparoscopic and General Surgery
Perth, Western Australia
Perth, Western Australia
Practice Details
Suite 12, Waikiki Specialist Centre,
221 Willmott Drive, Waikiki WA 6169
Please call (08) 9592 2298 for an appointment.
Fax: (08) 6314 1524
or email us
Office hours
9am–4pm Monday to Friday
Affiliations



© 2022 Perth General Surgery.
All Rights Reserved. Content and images on this website are subject to copyright.