Pilonidal Sinus Disease
This is a skin and subcutaneous (‘fat layer under the skin’) condition that affects the natal cleft (the area over the tail bone).
A pilonidal sinus is a sinus tract (small communication tract) that connects the skin of the natal cleft (area between the buttock) and a focus of infection in the deeper tissues, which commonly contains hairs.
A pilonidal sinus is a sinus tract (small communication tract) that connects the skin of the natal cleft (area between the buttock) and a focus of infection in the deeper tissues, which commonly contains hairs.
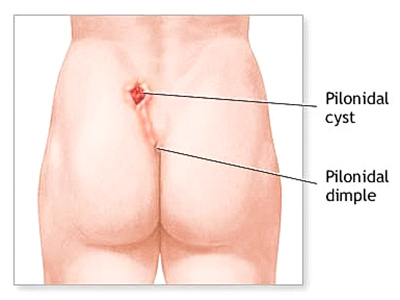
Location.

Clinical appearance.
Whilst the exact cause of the disease is uncertain, it is believed to be related to hair follicles / fragments and the shape of the natal cleft itself. This may be related to minor congenital abnormality of the area, which may explain why the condition may occur within family groups.

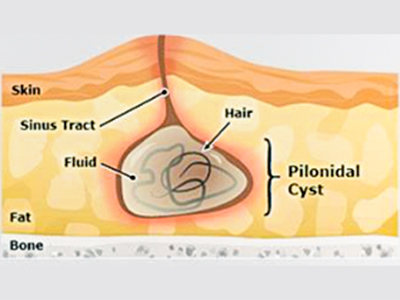
Pilonidal sinus anatomy.
Risk factors for the disease
Risk factors for the disease include:
- thick coarse body hair
- obesity
- prolonged sitting
- being male (more common than female), especially around puberty
- family history.
Symptoms
Pilonidal abscess
This is a collection of pus and hair fragments within the deeper tissue of the area. Patients will present with a painful and inflamed lump that may be accompanied by fever.
This will require surgical intervention, unless the abscess drained spontaneously.
This will require surgical intervention, unless the abscess drained spontaneously.
Pilonidal sinus
This consists of an opening(s) on the skin (This can be in midline or off the midline) through which pus and other discharge is seen. The discharge may be intermittent in nature. This may follow an abscess, but sometime can occur without a history of abscess. This condition may be chronic in nature.
Pilonidal cyst
This is a closed cavity with hair follicles and fluid. It is not infected.
Management
Pilonidal abscess
This will require antibiotics and ‘lancing’ (incision and drainage) of the abscess. This may be performed under local or general anaesthetics. The abscess is lanced and the pus and hair fragments removed. The wound is left open and packed with a dressing. Further dressing may be needed for a period of time—this is done in the community.
Pilonidal sinus
This will require excisional surgery or EPSiT.
This will require antibiotics and ‘lancing’ (incision and drainage) of the abscess. This may be performed under local or general anaesthetics. The abscess is lanced and the pus and hair fragments removed. The wound is left open and packed with a dressing. Further dressing may be needed for a period of time—this is done in the community.
Pilonidal sinus
This will require excisional surgery or EPSiT.
Surgery
Excisional surgery
The aim of the surgery is to completely excise all affected tissue—the external skin opening (sinus pits), fistulous tract and cavity. This is performed under general anaesthetic.
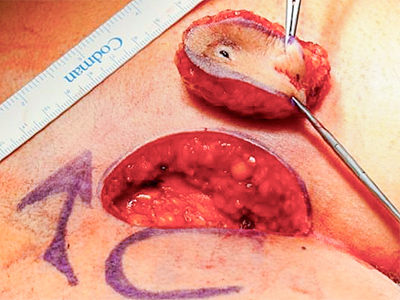
The resultant wound defect can be managed in one of three possible ways:
There are a number of flap reconstructions that may be used, such as advancement flap, rotational flap and Limberg flap. Mr Ahmad will discuss the flap reconstruction (using diagrams and photos during your consultation).
- Left open to heal from the base. Tissue will grow to fill the cavity. During this period, regular community based dressings will be needed. The duration of this dressing may be months, dependent on the size of the wound.
- Direct primary closure of the wound. The wound is closed with sutures. Due to mobility of the area, the sutures may ‘cut out’, in which case the wound may then be managed as option (1) above.
- Closure with flap reconstruction (see below). Most patients with a chronic or recurrent pilonidal disease will require excisional surgery with flap reconstruction. The principal objectives are to excise all affected tissue and ‘flatten out’ the natal cleft.
There are a number of flap reconstructions that may be used, such as advancement flap, rotational flap and Limberg flap. Mr Ahmad will discuss the flap reconstruction (using diagrams and photos during your consultation).
Endoscopic Pilonidal Sinus Treatment (EPSiT)
This is a video assisted treatment for the treatment of the pilonidal sinus and its recurrences.
A small scope is placed through the pilonidal sinus opening. The pilonidal sinus tract is then visualised and any hair fragment or debris is removed. The tract lining is then destroyed, either with mechanical equipment or diathermy (burning with electrical current). The sinus tract is then either left open to granulate spontaneously or filled with surgical glue or biodegradable mesh.
A small scope is placed through the pilonidal sinus opening. The pilonidal sinus tract is then visualised and any hair fragment or debris is removed. The tract lining is then destroyed, either with mechanical equipment or diathermy (burning with electrical current). The sinus tract is then either left open to granulate spontaneously or filled with surgical glue or biodegradable mesh.
The EPSiT advantages
- Direct vision of the tract allows the surgeon to accurately identify the anatomy of the disease and allows the complete removal of the hairs and their follicles.
- The aesthetic result is excellent with no deformity to the buttock area. The resultant hole is typically the same size as the presenting sinus opening. There is no large incision and therefore there is no large scar.
- There is no need for painful dressings for long period of time.
- There is shorter less intrusive recovery. The procedure can be done either as a day procedure or with just an overnight stay. Most patients will be able to return to normal activities after a few days.
- The patient’s quality of life is better compared to the traditional techniques.
Complications
Potential complications of the surgery are:
General complications of surgery
This includes allergic reaction to the drugs used, Deep Venous Thrombosis (DVT) and chest infection.
Specific complications of pilonidal surgery
Wound infection, haematoma (blood clot within operative site), seroma (accumulation of clear non infected fluid), wound dehiscence (break down).
Recurrence of disease (5–15 %). Further surgery may be needed.
For EPSiT—wound infection, bleeding/haematoma, recurrence, repeat procedure/need for a different procedure.
General complications of surgery
This includes allergic reaction to the drugs used, Deep Venous Thrombosis (DVT) and chest infection.
Specific complications of pilonidal surgery
Wound infection, haematoma (blood clot within operative site), seroma (accumulation of clear non infected fluid), wound dehiscence (break down).
Recurrence of disease (5–15 %). Further surgery may be needed.
For EPSiT—wound infection, bleeding/haematoma, recurrence, repeat procedure/need for a different procedure.
Postoperative management
Postoperative details
A patient undergoing incision and drainage of pilonidal abscess may be able to go home on the same day of surgery. On-going community based dressing will be required.
Patients undergoing excisional surgery may be required to stay as an inpatient for a few days. If the resultant wound is left open, it will required to be dressed on a regular basis in the community.
The patient is strongly encouraged to organise at least 2 weeks off work (less for EPSiT).
Patients undergoing excisional surgery may be required to stay as an inpatient for a few days. If the resultant wound is left open, it will required to be dressed on a regular basis in the community.
The patient is strongly encouraged to organise at least 2 weeks off work (less for EPSiT).
Post Discharge management
The patient will be discharged with analgesia and antibiotics.
Mr Ahmad’s Post Op Care Consultant will contact the patient 3–4 days after discharge.
A follow-up appointment will be made during the consultant’s review.
Also please see: Post discharge (in Surgery Process)
Mr Ahmad’s Post Op Care Consultant will contact the patient 3–4 days after discharge.
A follow-up appointment will be made during the consultant’s review.
Also please see: Post discharge (in Surgery Process)
Things to be aware of
If you:
please contact Mr Ahmad’s rooms on 9592 2298.
- have increasing pain from the wound
- have discharge from the wound
- have wound breakdown
- are feeling unwell
- or have any other concern,
please contact Mr Ahmad’s rooms on 9592 2298.
Clinical Associate Professor Hairul Ahmad MBBS FRACS
Upper Gastrointestinal, Advanced Laparoscopic and General Surgery
Perth, Western Australia
Perth, Western Australia
Practice Details
Suite 12, Waikiki Specialist Centre,
221 Willmott Drive, Waikiki WA 6169
Please call (08) 9592 2298 for an appointment.
Fax: (08) 6314 1524
or email us
Office hours
9am–4pm Monday to Friday
Affiliations



© 2022 Perth General Surgery.
All Rights Reserved. Content and images on this website are subject to copyright.