Anal fistula disease
An anal fistula is a tract connecting the inside of anal canal (back passage) and the skin.
Causes
Commonly anal fistula results from an abscess that has either spontaneously drained through the skin or drained surgically.
A small percentage of patients may present with a fistula without a history of abscess.
A small percentage of patients may present with a fistula without a history of abscess.
Anatomy of the fistula
There are different types of anal fistula, depending on the route of the communication tract.
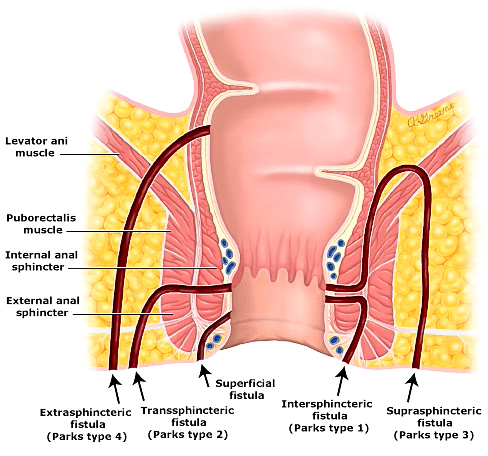
Anal fistula anatomy
Symptoms
A patient with an abscess typically present with pain and swelling. There may also be associated fever and feeling generally unwell.
A patient with fistula will have ongoing discharge from an opening in the skin. This may be bloodied, pussy or faecal stained.
A patient with fistula will have ongoing discharge from an opening in the skin. This may be bloodied, pussy or faecal stained.
Investigations
A patient may require a MRI examination of the area to define the fistula anatomy.
Management
A patient with an abscess will require that the abscess be drained as an emergency.
The management of an anal fistula will depend on whether the sphincter muscle is involved.
The management of an anal fistula will depend on whether the sphincter muscle is involved.
Surgery
Options include:
Cutting open the fistula (Fistulectomy)
This is done when the fistula does not involve or involve the lower part of the sphincter muscle.
The skin over the fistula and fistula tract is cut open. The wound is left open to slowly heal. Regular dressing may be needed.
The skin over the fistula and fistula tract is cut open. The wound is left open to slowly heal. Regular dressing may be needed.
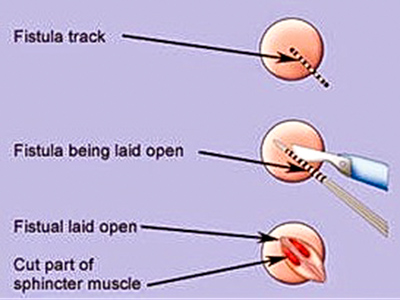
Fistulectomy
Seton placement
This a special 'suture' that is placed through the fistula tract to allow for drainage of any pus.
This is used specifically for fistula that involve the high part of the sphincter. The seton is then adjusted with time in planned operative protocol.
This is used specifically for fistula that involve the high part of the sphincter. The seton is then adjusted with time in planned operative protocol.
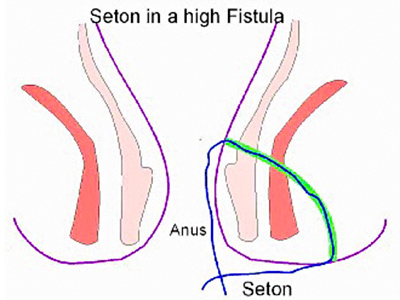
Seton placement
Mesh plug / surgical glue
In this method, the communicating tract is filled with a mesh plug or surgical glue.
Video Assisted Anal Fistula Treatment (VAAFT)
This is a new method, where the fistula tract is visualised and inspected using a small rod-shaped camera (video-scoped).
The tract is then cleaned and mesh plug or glue placed into the tract.
The tract is then cleaned and mesh plug or glue placed into the tract.
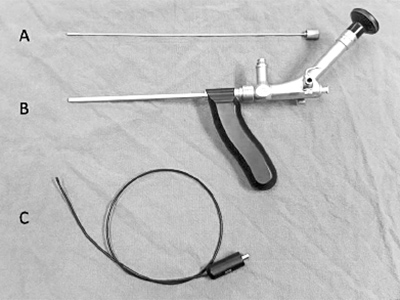
VAAFT equipment

VAAFT method
Complications of anal fistula management
The complications are heavily influenced by the complexity of the fistula disease, the extent of the sphincter muscle involvement and the nature of the surgery.
In general, the complications include the following and will be discussed in more detail during the consultation:
In general, the complications include the following and will be discussed in more detail during the consultation:
- Bleeding (haematoma)
- Wound infection
- Incontinence – this risk may occur when the sphincter muscle is damaged. The risk will depend on the type of procedure being performed.
- Recurrence – The recurrence rate will depend on the complexity of the disease and the type of procedure performed.
Postoperative management
This depends on the type of procedure being performed.
It varies from a few days of post-operative time off for VAAFT with minimal dressing requirement to regular outpatient dressing requirement with a fistulectomy. A seton placement procedure will require a number of planned operative visits.
It varies from a few days of post-operative time off for VAAFT with minimal dressing requirement to regular outpatient dressing requirement with a fistulectomy. A seton placement procedure will require a number of planned operative visits.
Clinical Associate Professor Hairul Ahmad MBBS FRACS
Upper Gastrointestinal, Advanced Laparoscopic and General Surgery
Perth, Western Australia
Perth, Western Australia
Practice Details
Suite 12, Waikiki Specialist Centre,
221 Willmott Drive, Waikiki WA 6169
Please call (08) 9592 2298 for an appointment.
Fax: (08) 6314 1524
or email us
Office hours
9am–4pm Monday to Friday
Affiliations



© 2022 Perth General Surgery.
All Rights Reserved. Content and images on this website are subject to copyright.