Vasectomy
Vasectomy is a proven permanent contraceptive method for men.
The spermatic tubes that carry sperm from the testicles are cut.
This procedure should be regarded as permanent. Even though reversal is possible, there is no guarantee of restoration of fertility. Both the patient and his partner need to accept the finality of the procedure.
After vasectomy, a man’s libido and sexual ability is unchanged. He is able to have an erection as before surgery. His ability to ejaculate is also unchanged.
The patient needs to be aware that a vasectomy does not protect him from sexually transmitted diseases (STD). A condom should always be used in certain situations.
The patient has to be aware of other methods of contraception. This includes abstinence, condoms, the oral contraceptive pill (for females) and intrauterine devices (IUDs) (for females).
The spermatic tubes that carry sperm from the testicles are cut.
This procedure should be regarded as permanent. Even though reversal is possible, there is no guarantee of restoration of fertility. Both the patient and his partner need to accept the finality of the procedure.
After vasectomy, a man’s libido and sexual ability is unchanged. He is able to have an erection as before surgery. His ability to ejaculate is also unchanged.
The patient needs to be aware that a vasectomy does not protect him from sexually transmitted diseases (STD). A condom should always be used in certain situations.
The patient has to be aware of other methods of contraception. This includes abstinence, condoms, the oral contraceptive pill (for females) and intrauterine devices (IUDs) (for females).
Anatomy
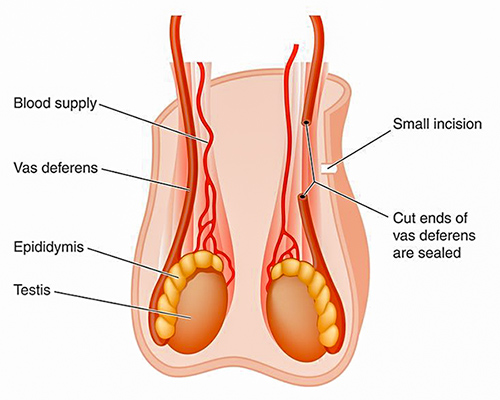
The spermatic tubes that carry sperm from the testicles are cut.
Indications
Indications for Vasectomy are:
- A patient who is sexually active.
- A patient that is certain that he no longer desires any more children. This decision should have been discussed thoroughly with his partner. The patient should be aware of the impact of his decision if his familial circumstances change in the future.
- The patient is aware of the implication of the surgery, especially the permanent nature of vasectomy.
Preoperative Preparation
The patient should have a shower the morning of the operation day and wash his genital area thoroughly with soap.
Arrangements need to be made for another person to drive the patient home.
Arrangements need to be made for another person to drive the patient home.
Surgery
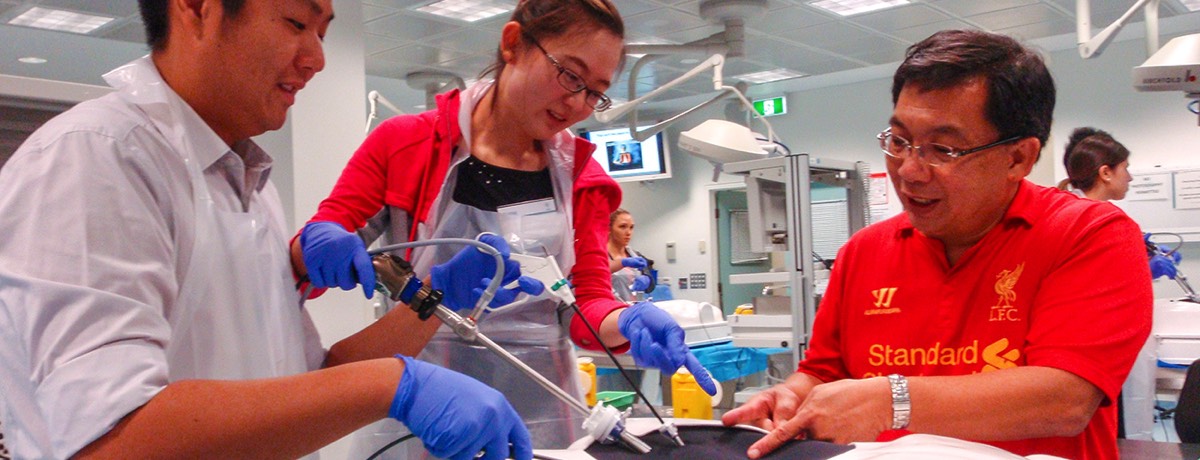
The procedure can be done under local anaesthetic or general anaesthetic.
A small incision is made in the scrotal skin. The spermatic duct is identified and brought through the skin. A segment of the duct is then removed.
The two ends of the duct are then tied. The skin is closed with dissolvable sutures. A repeat procedure is then performed on the other side.
A small incision is made in the scrotal skin. The spermatic duct is identified and brought through the skin. A segment of the duct is then removed.
The two ends of the duct are then tied. The skin is closed with dissolvable sutures. A repeat procedure is then performed on the other side.
Complications
- Early failure (0.2%)
- Long term failure (1/3000–7000)
- Haematoma (2%)
- Infection
- Congestion orchitis
- Chronic orchalgia (<1%)
- Sperm granuloma
- Antibodies to sperm. This can develop after vasectomy. These antibodies can inactivate sperm, reducing the chance of fertility after a vasectomy reversal.
Postoperative management
- The patient is encouraged to wear fitting supportive underwear.
- The patient should take pain relief as directed. A script for oral pain relief will be given on discharge from hospital.
- The Post Operative Care Consultant will contact the patient a few days post discharge.
- Sexual activities can resume when the patient is comfortable physically. However please note the Special Warning.
Special Warning
Vasectomy does not render a patient immediately infertile.
Other methods of contraception must be used until a semen analysis (done at 10 weeks after the vasectomy and at least 20 ejaculations) confirms the infertility.
Other methods of contraception must be used until a semen analysis (done at 10 weeks after the vasectomy and at least 20 ejaculations) confirms the infertility.
Clinical Associate Professor Hairul Ahmad MBBS FRACS
Upper Gastrointestinal, Advanced Laparoscopic and General Surgery
Perth, Western Australia
Perth, Western Australia
Practice Details
Suite 12, Waikiki Specialist Centre,
221 Willmott Drive, Waikiki WA 6169
Please call (08) 9592 2298 for an appointment.
Fax: (08) 6314 1524
or email us
Office hours
9am–4pm Monday to Friday
Affiliations



© 2022 Perth General Surgery.
All Rights Reserved. Content and images on this website are subject to copyright.